You have successfully logged out.
Not registered yet?
Air Embolism
The causes of venous air embolisms are preventable
Read how health care professionals can reduce the risk significantly and why this is a particularly important task in paediatrics.
Medical Professional
This information is meant for medical professionals only. Please confirm that you are a medical professional before accessing the information.
Confirm Yes, I am a health care professional. Cancel No, I am not a health care professional.What is an Air Embolism?

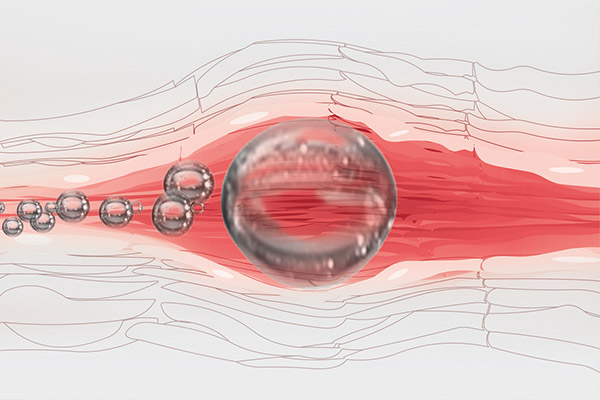
An air embolism or a gas embolism is principally caused by the entry of air bubbles into the vascular system, leading to a blood vessel blockage and, therefore, to systemic effects.2, 3
Air embolisms can occur due to:
- Open IV systems, e.g., through accidental leakage.
- Parallel infusions.
- Improperly primed infusion lines.
The amount of air entry is influenced by the position of the patient. In an upright position, the risk increases the higher the vein is above the heart level.3, 4, 5
Gravity infusions and infusion pumps connected together can lead to beading effects (fluid–air–fluid, etc.) when the gravity infusion runs dry.6 Furthermore, the incorrect handling of pressure infusion procedures poses a risk of air embolism.7, 8
Why is an Air Embolism a Risk in Paediatrics?
In children and especially preterm babies and neonates, the smallest amount of air can lead to an air embolism with fatal consequences.9 Paediatric and neonatal patients suffering from a persistent foramen ovale (PFO) or patent ductus arteriosus (RDA) are particularly affected. If air passes through the PFO or RDA, there is also a risk of a systemic (arterial) air embolism in addition to the risk of a venous air embolism.10
The effects of small total volumes of air can be physiological changes, such as:10
- Mechanical pulmonary vascular obstruction
- Pulmonary vasoconstriction
- Hypoxemia
- Increased airway resistance
- Decreased lung compliance
- Myocardial ischemia
In paediatric neurosurgery, a venous air embolism (VAE) is more common when the head is above heart level, such as in the sitting position. The incidence of these cases in children has been reported to be as high as 33%.10,11
Air entrainment is dependent upon the magnitude of the negative pressure developed between the site of entry and the right heart. Therefore, the sitting position represents a particular risk for an air embolism. Air entry is also possible in other surgical positions if the potential for a negative pressure gradient exists.10
In addition to neurosurgery, air emboli have also been reported in children during the diagnostic radiological procedures arthrography, arteriography, cisternal air myelography and pneumoencephalography.10

How to Reduce the Risk of an Air Embolism in Children?
In paediatrics, prevention or rapid treatment of an air embolism is extremely important. Close monitoring is crucial to prevent air entry until a critical air volume causes disastrous physiological derangements.10
Ensuring whenever possible that the patient is in a position where the affected vein is located below the level of the heart helps to reduce the risk. The Trendelenburg or supine position is preferable for the application of central venous catheters.3, 4
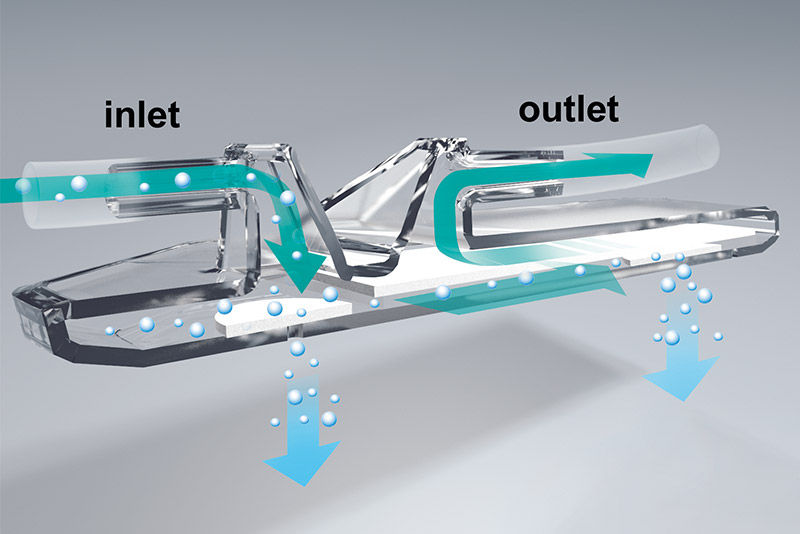
An air separator close to the patient access reduces the risk of air embolism during infusion. Two 0.02 µm hydrophobic PTFE membranes prevent air embolism regardless of the position of the inline IV filter.12,13
Functionality of an IV filter to prevent air embolism.
Three-way stopcocks in the bypass placed in the ascending siphon tube should be used in parallel infusions. For gravity infusions, use check valves.
Last but not least, modern infusion sets with an air stop mechanism also help to minimise air embolism.
Highlight Safety Products
Risk Prevention in Paediatrics & Neonatology
[1] Ho AMH. Is Emergency Thoractomy Always the Most Appropriate Immediate Intervention for Systematic Air Embolism After Lung Trauma? Chest. 1999;116(1):234-7.
[2] McCarthy C, Behravesh S, Naidu S, Oklu R. Air Embolism: Practical Tips for Prevention and Treatment. Clin Med. 2016;5(11):93.
[3] Cook LS. Infusion-related air embolism. J Infus Nurs 2013;36(1):26-36.
[4] Gabriel J. Infusion therapy. Part two: Prevention and management of complications. Nurs Stand 2008;22(32):41-8.
[5] Lee PT, Thompson F, Thimbleby H. Analysis of infusion pump error logs and their significance for health care. Br J Nurs 2012;21(8):12-20.
[6] Obermayer A. Physikalisch-technische Grundlagen der Infusionstechnik – Teil 2. Medizintechnik 1994;114(5):185-190.
[7] Zoremba N, Gruenewald C, Zoremba M, Rossaint R, Schaelte G. Air elimination capability in rapid infusion systems. Anaesthesia 2011;66(11):1031-4.
[8] Suwanpratheep A, Siriussawakul A. Inadvertent venous air embolism from pressure infuser bag confirmed by transesophangeal echocardiography. J Anesthe Clinic Res 2011;2(10).
[9] Levy I, Mosseri R, Garty B. Peripheral intravenous infusion – another cause of air embolism, Acta Paediatr. 1996 Mar;85(3):385–6.
[10] Porter SS, Boyd RC, Albin MS. Venous air embolism in a child undergoing posterior fossa craniotomy: a case report. Can Anaesth Soc J. 1984 Jan;31(1):86-90.
[11] Sriganesh K, Mittal M, Jadhav T. Venous Air Embolism. Journal of Neurosurgical Anesthesiology 2016 Jan;28(1):85-6.
[12] Phillips LD, Gorski LA. Infusion equipment – filters. In: Phillips LD, Gorski LA. Manual of I.V. therapeutics – evidence-based practice of infusion therapy. Philadelphia: Davis Company. 2014;265-268.
[13] Hadaway L. Infusion therapy equipment – Infusion filter. In: Alexander M. Infusion Nurses Society.Infusion nursing - an evidence-based approach. Philadelphia, Pa. [u.a.]: Saunders Elsevier. 2010;403-407.





