You have successfully logged out.
Not registered yet?
Wound Management
Remove barriers to wound healing. In every sense.
Even a minor injury can turn into a chronic wound. That is why the success of wound treatment depends on the condition of the wound, the preparation of the wound bed and the correct choice of dressing besides other factors. B. Braun offers a holistic approach to wound management which includes wound infection management, exudate management and skin care.
Medical Professional
This information is meant for medical professionals only. Please confirm that you are a medical professional before accessing the information.
Confirm Yes, I am a health care professional. Cancel No, I am not a health care professional.Help to minimise the risk of wound infections
Chronic wounds get not only colonised by pathogens, like bacteria but can also become infected. This compromises not only the normal healing process but may impact patient’s quality of life. Even minor wounds can lead to fatal sepsis.
Learn how to manage wound infections
Prevention and management of wounds
A holistic approach
Manage biofilm
Biofilms can be difficult to detect. But biofilm is undoubtedly a key factor of chronic wound infection and delayed wound healing.
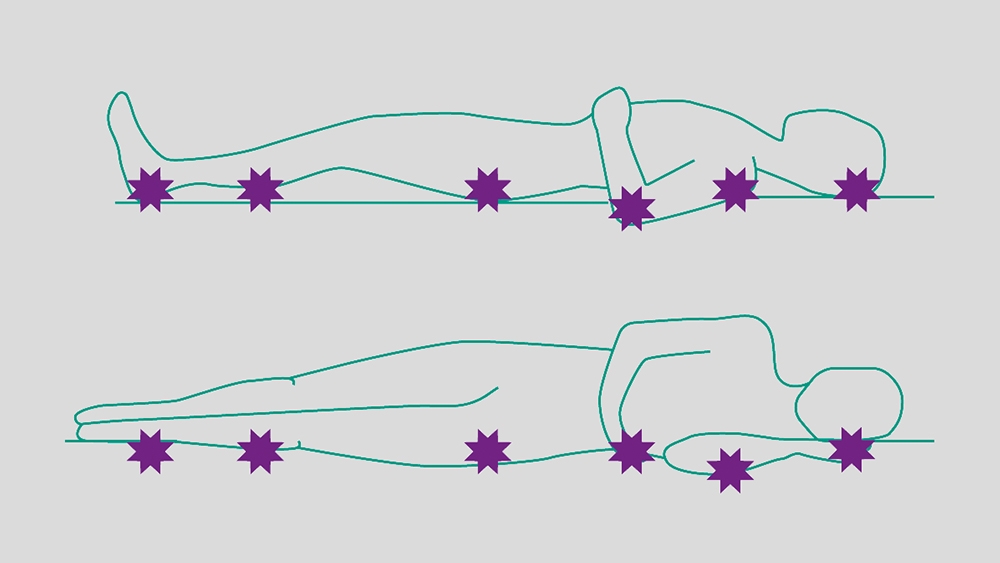
Manage pressure injuries
Pressure ulcers are frequent. They can develop quickly, and they are associated with substantial health burden. But: The occurrence of pressure injuries can be minimised with the help of a holistic approach.

Manage burns efficiently
Anyone can suffer from a burn and depending on its severity, different treatment concepts are required. B. Braun has specialized in the management of severe burns.
Learn more about the management of burnsOur services
Know-how and guidelines for wound management specialists
Wound Management
It will be forwarded to a responsible contact person who will get in touch with you as soon as possible.
Your request could not be submitted. Please try again.
warningStay connected with My B. Braun
With your personalized account, your online experience will be easier, more comfortable and safe.









